With cancer costs in the USA spiralling into many tens of thousands of dollars1, and costs of some new biological treatments approaching £100,000 2, you could be forgiven for overlooking cancer interventions in developing countries as too expensive to be cost-effective.

Not so, according to the 2015 Disease Control Priorities 3rd Edition (DCP3)3.
The document details cost-effective cancer intervention and treatment strategies, offering an “Essentials Cancer Intervention Package” designed to reduce deaths from cancer, tailored to the wealth of a country and the infrastructure available. The 2011 World Health Organisation (WHO) “Best Buys” document4 also details highly cost-effective strategies for cancer intervention which could save millions of lives in the coming century, and which require relatively little infrastructure.
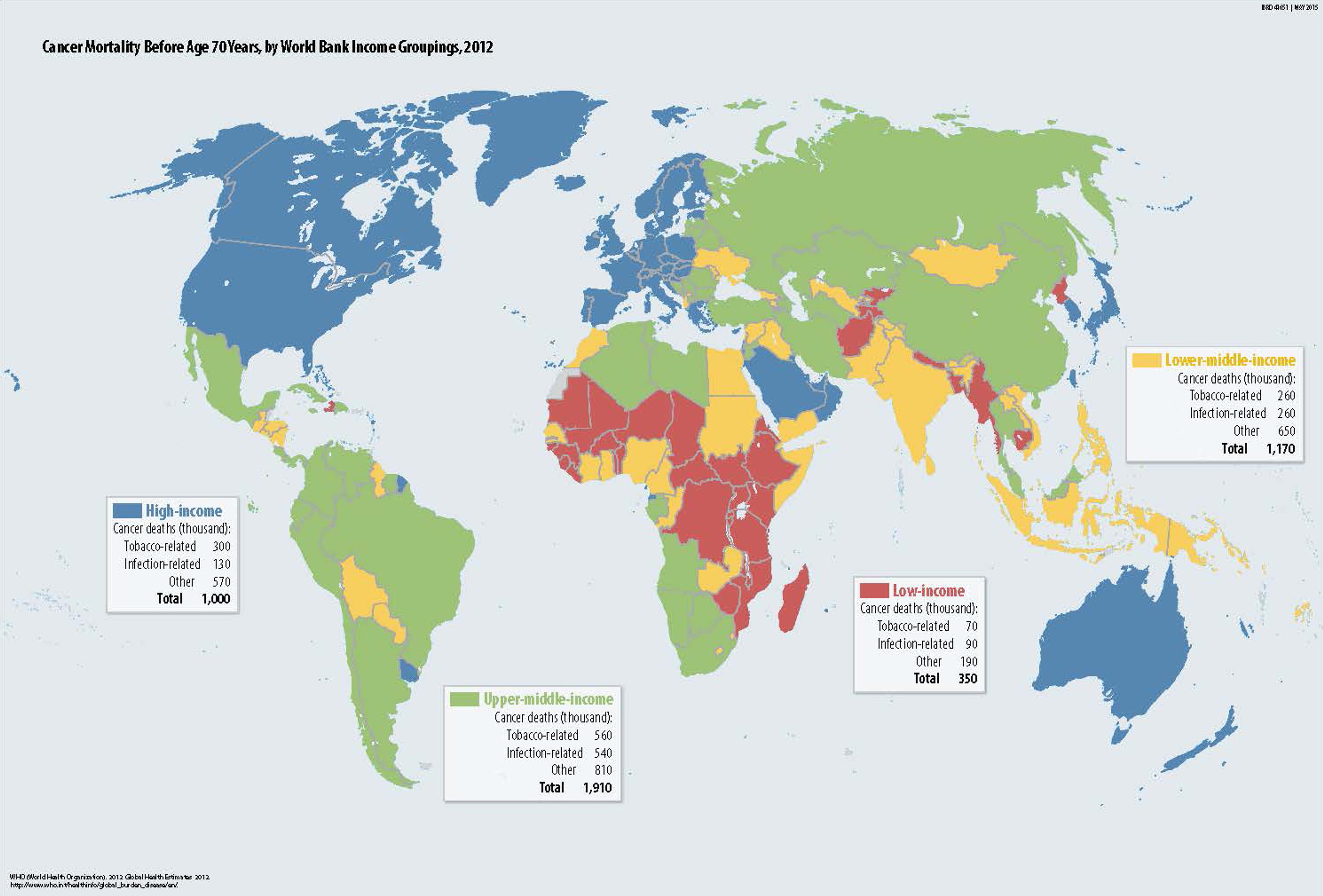
Cancer incidence worldwide - DCP-3 cancer report
Tobacco
Tobacco-related deaths are increasing rapidly, especially in low and middle income countries (LMICs)5 6, and tobacco use threatens to kill far more in the coming decades than it has in the past. By the middle of this century, it has been estimated that tobacco-related deaths will reach 10 million per year7.
With up to 2/3 of smokers dying of smoking-related diseases8 and losing, on average, 10 years of life (DCP3)9, it’s hardly surprising that both the WHO and DCP3 recommend tobacco intervention as one of their top global health priorities. In 2013, the World Health Assembly introduced a target for tobacco control 10, calling for a 1/3 reduction in use by 2025, with the aim of saving 200 million lives.
Tax boosts to increase cigarette price have been shown to reduce smoking, especially amongst young people 11 12 13 14. A report by the World Bank estimated that for every 10% increase in cigarette cost, tobacco consumption would drop by 4% in high income countries (HICs) and 8% in low income countries (LICs). Young people are also more likely to quit and less likely to start when prices are high15.
The WHO therefore recommends that excise taxes should account for 70% of cigarette cost16. A report by the Asian Development Bank stated that increasing the price of cigarettes by 50% through taxation would avert 27 million tobacco-related deaths in China, India, Thailand, the Philippines and Vietnam alone17. Price increases hit the poorest smokers in a population hardest but the taxes are not considered to be regressive since those with low income are the most likely to quit and gain the intended health benefits (for more information on this see our blog post - “Is Tobacco Control a “Best Buy” for the Developing World)18 19 20.
Alongside price increases, education is also vital. The WHO Global Adult Tobacco Survey for China showed that only 23% of Chinese adults knew that smoking caused lung cancer, heart attacks and strokes21. This lack of awareness affects the poorest in a population the most, with those who are illiterate unable to read warning labels.
Pictorial warnings have been used to try and re-balance this inequality in some countries22, and there is evidence that pictorial warnings improve awareness of dangers of smoking and reduce the number of young people starting 23. Packaging controls are also important in reducing the impression that some cigarette brands are less harmful than others 24.
Total advertising bans have been effective in reducing cigarette consumption25 26, especially in low/middle income countries (LMICs)27, and bans on smoking in the workplace have also been shown to reduce consumption 28 29.
Large investments from The Bill and Melinda Gates Foundation and Bloomberg Philanthropies have gone towards increasing awareness of the dangers of tobacco, funding research and collecting data, and pushing for changes in policy to reduce tobacco use30 31.
For more on tobacco control, check out this blogpost and this overview by GiveWell.
Liver Cancer
Liver cancer has one of the highest mortality rates of any primary cancer. In 2012, it caused 746,000 deaths out of 782,000 cases 32. Highly cost-effective interventions are available to reduce the number of people who get the disease, and these interventions are recommended by both WHO and DCP3.
Hepatitis B vaccination is the first line of defence. Hep B is a cancer-causing virus responsible for around 60% of hepatocellular carcinoma (the most common type of liver cancer) in LICs 33. The virus attacks the liver, sometimes setting up an infection which can last for years. 15-45% of those with long-term infection will develop serious complications such as cirrhosis and liver cancer during their lifetime 34 35.
The majority of countries now aim to vaccinate children at birth, but coverage at birth is still low in some areas 36. Initial vaccination within 24 hours is very important in preventing mother-child transmission, which often results in dangerous long-term infection37 38. Increasing vaccine coverage should decrease Hep B infection rates and hence liver cancer incidence39. Our vaccination report has more information on the cost-effectiveness of vaccination. As with GiveWell’s vaccination report, Giving What We Can did not find any promising vaccination funding opportunities.
Targeting other region-specific causes of liver cancer may also be cost-effective. High rates of liver fluke infection occur in some areas of eastern Asia, especially within the Mekong River Basin in Southeast Asia, where around 40 million people are infected40 41. The worms can infect a host for many years, causing damage to the liver’s bile ducts which can eventually lead to cancer42. Treatment with Praziquantel can clear the infection, though people in the area are often quickly reinfected by eating raw fish dishes 40.
Liver flukes are not the only parasite to play a role in cancer. Infection with Schistosoma haematobium has long been associated with bladder cancer 43, and is recognised as a cause of cancer by the IARC 44 45. Studies in the 1970s and 80s noted that bladder cancer was more common in areas in which Schistosoma haematobium infection was common46 and biopsies of tumours showed high incidence of schistosome infection 47 48. This neglected tropical disease is easily and cheaply treatable, and two of Giving What We Can’s recommended charities - the Schistosomiasis Control Initiative and Deworm the World Initiative - can provide treatment for around $2 per person per year.
Poor food storage can also lead to higher rates of liver cancer. Aspergillus flavus and Aspergillus fumigatus can infect staple foods during cultivation, including peanuts, rice and corn49. In areas where these foods are then stored in warm, high humidity environments, the fungus is able to grow, producing the highly potent aflatoxin. This toxin causes DNA mutations and is associated with both liver and lung cancer.
In people with chronic Hep B infection, exposure to aflatoxin increases the chance of liver cancer by 30-fold. Improved grain storage and cultivation methods can reduce the amount of the toxin that people consume, and with 4.5 billion people currently exposed to aflatoxin, the potential for reducing suffering is enormous.
Cervical cancer
The final WHO “Best Buys” are designed to reduce deaths from cervical cancer. Screening and treatment for early cervical lesions have been shown to be cost-effective. Opportunistic screening with an acetic acid test is low-cost and cancerous/precancerous lesions can be removed on the same day 50 51.
Since high-risk strains of Human Papilloma Virus (HPV) are responsible for up to 98% of cervical cancer cases 52 53, HPV screening can also be highly effective in averting deaths from cervical cancer. Screens are low-cost and some can be done at home, so women who do not want to come to the clinic or undergo a cervical examination can still be screened 54.
Vaccination against HPV virus strains 16 and 18 (those most commonly associated with cervical cancer) is also highly cost-effective in some areas55. These vaccinations are included in the DCP3 recommendations, though not the WHO “Best Buys” list. HPV-16 and -18 are responsible for more than 70% of cervical cancers 56, with HPV-16 detected in 57% of cervical cancers and HPV-18 detected in 17% 57. Along with 6 less common strains, these HPV types are responsible for over 90% of cervical cancer cases.
The HPV vaccine is relatively high-cost and requires two follow-ups, so it’s not cost-effective in all areas. However, heavily subsidised vaccines, such as those offered by GAVI alliance, make vaccination much more cost-effective (vaccines at $5 per dose are available to 37 countries in Sub-Saharan Africa)58.
The vaccine requires a cold chain, making some areas of sub-Saharan Africa difficult to cover, but it has been estimated that 70% coverage of 9-year old girls for 5 years could avert 670,000 cases of cervical cancer in the region59.
Breast cancer
Included in the DCP3, but not the WHO recommendations, is screening for breast cancer and treatment of early-stage tumours. Since presentation with advanced-stage tumour is more common in low/middle income countries60, examination by medical professionals and education in breast self-awareness may decrease death rates, as treatment earlier in the disease course is easier and has a higher success rate61.
A case study in Malaysia found that incidence of patients presenting with late stage breast cancer decreased from 77% to 37% after a country-wide drive to increase awareness. As part of the drive, nurses began to visit rural areas to give talks, demonstrate breast awareness and perform examinations62.
Childhood cancers
Finally, DCP3 also highlights the cost-effectiveness of treating some childhood cancers. The very high cure rates seen in some childhood cancers in HICs are often dependant on intensive supportive care which is not available in LICs63. However, some studies have shown less intensive treatments of certain cancers to be effective and highly cost-effective, with treatment of Burkitt’s Lymphoma, for instance, costing as little as £500 64 65 66 67.
Twinning programs, linking hospitals in LICs with specialist hospitals in HICs allow expertise to be shared, improving treatment and survival rates68. The success seen in childhood cancer can act as a strong motivator to encourage governments to pursue cancer treatment programs and give early stage patients the hope required to seek help as soon as they discover symptoms of disease3.
Conclusion
Despite the high cost of cancer in HICs (£5.8bn in the UK in 2010/11 - 5.4% of NHS budget69), affordable changes can be made in LICs which might avert millions of deaths over the coming century. In many cases, prevention is far more cost-effective than treatment. However, perhaps surprisingly, in cases such as cervical cancer, and potentially some childhood cancers, treating early stage disease is also highly cost effective.