Cancer (Part 1 of 2)
Giving What We Can no longer conducts our own research into charities and cause areas. Instead, we're relying on the work of organisations including J-PAL, GiveWell, and the Open Philanthropy Project, which are in a better position to provide more comprehensive research coverage.
These research reports represent our thinking as of late 2016, and much of the information will be relevant for making decisions about how to donate as effectively as possible. However we are not updating them and the information may therefore be out of date.
Cause Area: Cancer
1. What is cancer?
Cancer is a collection of related diseases, all of which involve the uncontrolled division of cells within the body.[^fn-1] These cell growths, also referred to as neoplasms, can spread to surrounding tissues and the rest of the body. Many common cancers can be treated, particularly if they are detected quickly, through methods such as radiotherapy, chemotherapy, and surgery. Many cancers can also be prevented by reducing or eliminating exposure to external agents, such as carcinogens found in tobacco smoke.1
2. How does it affect people?
Worldwide, cancer is a major contributor to both mortality and morbidity. Each year, approximately 14 million new cases are recorded,2 along with 8.24 million deaths attributable to cancer.34 This equates to approximately 8% of disability-adjusted life years (DALYs incurred) and approximately 15% of all deaths.5 See Figure 1 below for a breakdown of how different types of cancer contribute to this total.
| Type of cancer | Annual deaths6 | Percentage of total deaths7 | Percentage of total DALYs8 |
|---|---|---|---|
| Lung | 1,590,000 | 2.99 | 1.42 |
| Liver | 745,000 | 1.49 | 0.85 |
| Stomach | 723,000 | 1.53 | 0.73 |
| Colorectal | 694,000 | 1.41 | 0.65 |
| Breast | 521,000 | 0.86 | 0.54 |
| Oesophageal | 400,000 | 0.80 | 0.40 |
Figure 1: Deaths and DALYs incurred, by type of cancer.
Cancer is commonly thought of as “...a disease of the rich…”,9 and it is indeed true that it makes up a significantly larger proportion of deaths in richer countries (see Figure 2). Even in age-standardised figures, cancer accounts for a greater relative number of both deaths (24.93% compared to 12.45%) and DALYs (13.97% and 7.45%) in developed nations than in developing nations, and this difference holds across every available age group (0-5, 5-14, 15-49, 50-69, and 70+ years),10 although this difference may be partly explained by the comparatively high incidence of communicable, maternal, neonatal, and nutritional diseases in the developing world (26.6%, compared to 5.36% in the developed world).11
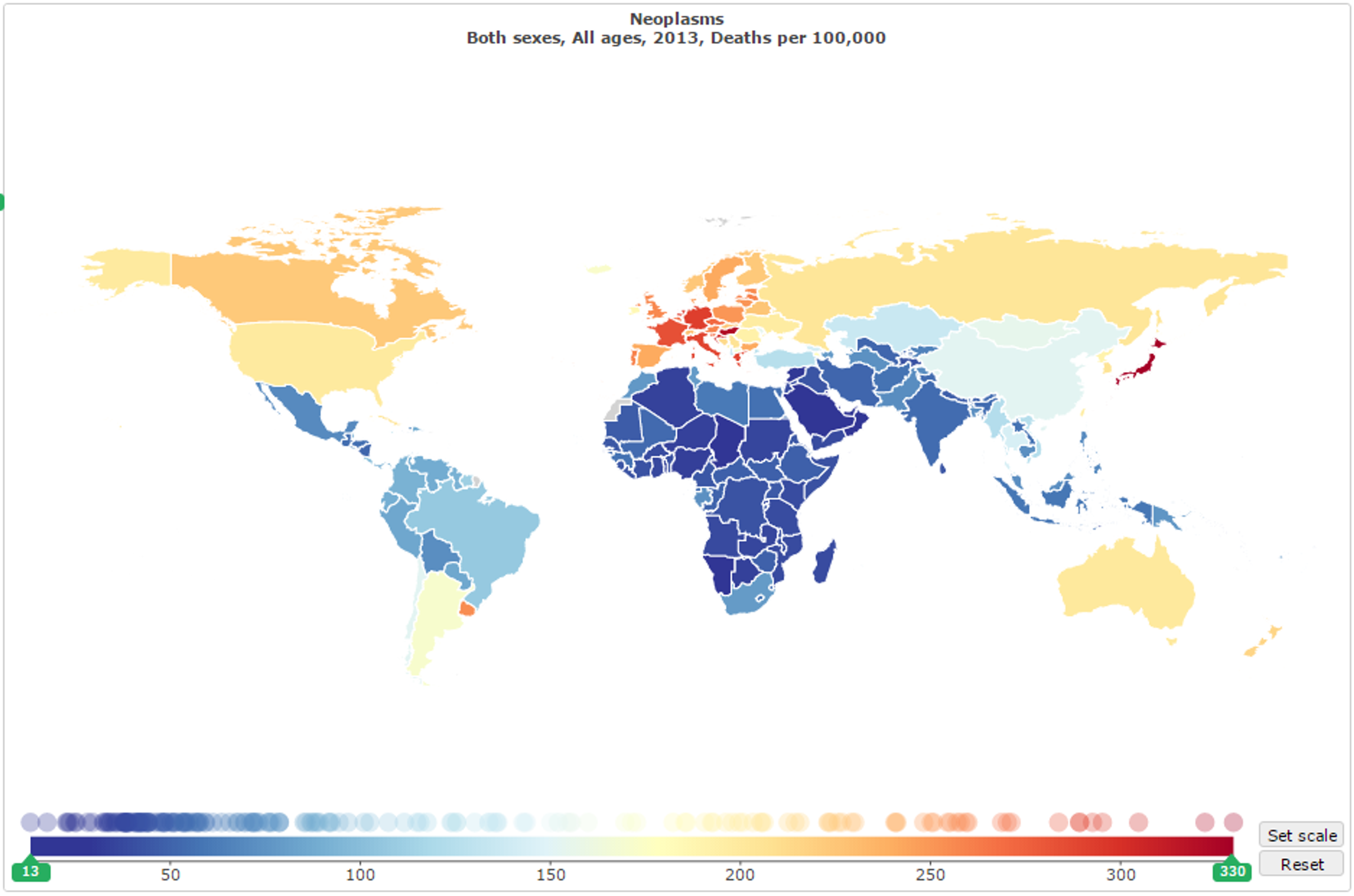
Figure 2: Residents of developed nations are, generally, more likely to die of cancer than those in developing nations.12
Still, most of the burden of cancer falls on the developing world. The World Health Organisation reports that more than 60% of new cancer cases occur in Africa, Asia, and Central and South America, due to their higher populations.13 Approximately 70% of all deaths attributable to cancer also occur in these regions14 and, in developing nations more widely, cancer accounts for 12.17% of all deaths (see Figure 3).15 This is potentially exacerbated by a lack of medical infrastructure, doctor training, and international funding for cancer treatment in the developing world.16
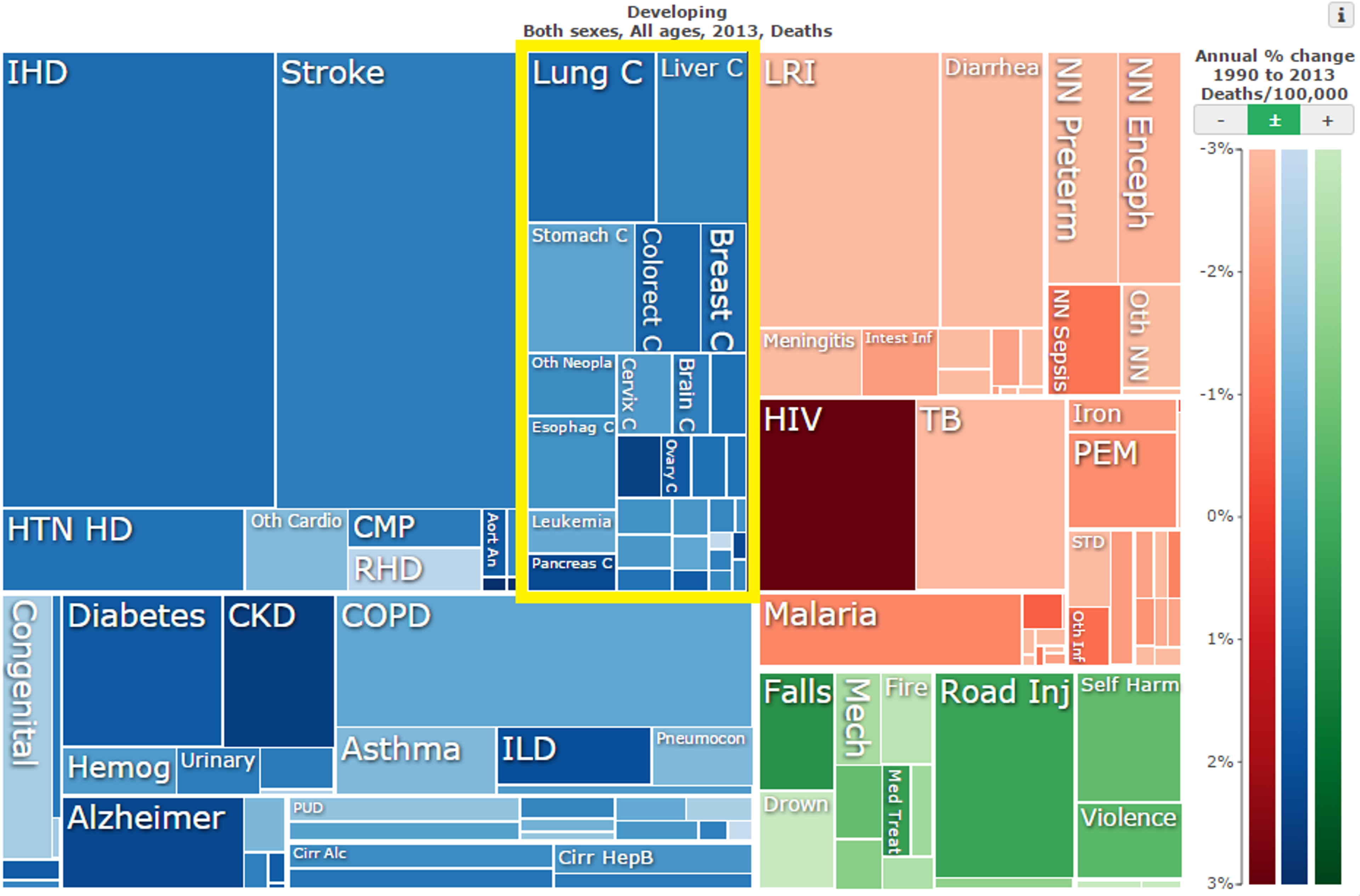
Figure 3: Neoplasms (outlined in yellow) as a proportion of total mortality in developing nations in 2013;17
Cancer predominantly affects older people, with the average years of potential life lost being comparatively small - only 12.5 years per cancer death,18 as opposed to diseases that affect infant mortality such as malaria. As a comparison against other diseases, cancer makes up only 11.3% of years of potential life lost despite causing 15% of all deaths. Thus, cancer incidence is therefore expected to increase as life expectancy increases. It is expected that the number of new cancer cases each year will rise by approximately 70% over the next two decades, resulting in 22 million new cases each year in 2034.19 At present, annual deaths due to cancer are growing approximately 50% faster in the developing world than in the developed world, and a large proportion of the additional mortality and morbidity can hence be expected to occur in developing nations.20
3. How can you address the problem?
Interventions to reduce mortality and morbidity due to cancer may be broadly categorised into: further research into the causes and treatment of cancer; activities which focus on the prevention of cancer cases; and the direct treatment of cancer. Another useful distinction is between interventions which focus on treating or preventing cancer in developed nations and those which focus their efforts on developing nations.
In this report, we recommend contributing donations towards interventions which focus on the prevention and treatment of cancer cases, specifically in developing nations. This is due to the more favourable cost-effectiveness of these areas in terms of $ per life saved, and their relative neglectedness.
4. Research
As the cancer burden is large, and also growing, if cancer research were successful in providing the means to prevent future deaths then its benefits would be enormous. Of the three types of cancer intervention identified in this report, research is the area for which the benefits can most easily be experienced by both developed and developing nations. New treatments and medicines which are discovered in one nation may later be used around the world.21
However, although the potential benefits of successful cancer research are very large and transferable across different nations, the area is already extremely well-funded relative to other diseases. Therefore, we do not recommend funding research as a means of reducing morbidity and mortality due to cancer. There already exist a variety of cost-effective methods to greatly reduce cancer cases (see the following sections).
Cancer research is very well-funded in comparison to other diseases. The National Cancer Institute in the United States has spent approximately $90 billion over the past 40 years on cancer research.22 As for charitable funding, there are 260 different nonprofit organisations in the US alone, with a combined annual budget of $2.2 billion.23 Even more impressively, pharmaceutical and biotechnology companies spend approximately $51.2 billion on research and development each year, with cancer a primary focus.24 Likewise,in the UK, spending on cancer research by the National Cancer Research Institute’s member organisations doubled between 2002 and 2010 to £500 million and has continued to grow.25 Although this makes sense due to the high prevalence of cancer in developed nations and hence the greater incentive to research cancer treatments, it is in sharp contrast to the $70 million of funding to developing countries to prevent deaths due to tobacco,26 and to the mere 10% of global research funding which is estimated to be allocated to those diseases (including Neglected Tropical Diseases such as schistosomiasis) which are specifically relevant to the poor and which cause the majority of the global disease burden.272829 Therefore, it is unlikely that donations to this area will have as high an impact as research into other areas, or as high an impact as direct action such as malaria prevention,30 deworming,31 development media,32 or tobacco control.33
Another major consideration is that there are a variety of cost-effective methods of cancer prevention already available and that it seems that further research into treatments (which dominates the field of cancer research) is unlikely to provide any methods of treatment which are more cost-effective than basic prevention. Research has already provided methods of diagnosis and treatment of early-stage cancers, as well as numerous highly effective prevention strategies such as tobacco control, Hepatitis B vaccination, breast cancer screening, and schistosomiasis treatment (see Section 5). However, when it comes to research into new treatments, even if a new drug were developed which completely cured a particular form of cancer, its sale price would likely be quite high given initial development cost of, on average, $2.6 billion34 as well as the financial interests of private companies which conduct the majority of cancer research and drug development. This has also been demonstrated in practice - 12 out of the 13 new cancer drugs approved in the United States in 2012 cost more than $100,000 per year of therapy.35 In comparison, the Against Malaria Foundation, one of the top charities recommended by Giving What We Can, prevents the death of a child under the age of 5 for every $2,838 donated.36 For cancer specifically, it happens to be the case that tobacco control could potentially prevent a death for as little as $1462 (see Section 5.2 below) and existing micronutrient fortification charities currently provide the opportunity to prevent deaths from stomach cancer for $19,100 each, in addition to producing a multitude of other health benefits (see Section 5.1). Given the extremely low cost of these interventions and the consistently high cost of new cancer treatments, it seems quite unlikely that any type of cancer research or development of new treatments in the near future will reveal a more cost-effective intervention than those available for malaria or those already available for cancer prevention. Thus, cost-effectiveness alone may exclude cancer research from being an effective method to save lives through charitable donations.
Given its crowdedness, we do not recommend donating to research as an effective method of reducing mortality and morbidity due to cancer, nor an effective method of reducing mortality and morbidity overall.
5. Prevention
The World Health Organisation details highly cost-effective strategies (which they call “Best Buys”) to tackle cancer which could save millions of lives in the coming century, and which require relatively little infrastructure.37 These strategies focus primarily on the prevention of cancer cases, which is considered a significantly more cost-effective method to reduce both morbidity and mortality in this area, and include: tobacco control to reduce lung cancer incidence (see Section 5.1); vaccination and treatment of related diseases (see Section 5.2); screening and vaccination specifically against cervical cancer (see Section 5.3); as well as screening and awareness raising for breast cancer (see Section 5.4).
Cancer prevention is likely to be more cost-effective in developing nations. Like treatment, the cost of preventative interventions are likely to be substantially higher in developed nations due to higher costs and because much of the low-hanging fruit may already be funded by governments and charitable organisations (for example, the Centers for Disease Control and Prevention in the United States and Public Health England). Only 5% of global resources devoted to cancer - $320 billion in total each year (on both treatment and prevention) - are spent in developing countries despite their higher total disease burden.38
Interventions are also unlikely to be as tractable in developed countries, due to public awareness already being relatively high, screening already being performed on a large scale, and vaccines and treatment for those conditions which commonly lead to cancer already being widely available.3940 Combined with the minimal resources allocated to it, this establishes cancer prevention in the developing world as a relatively neglected area, as will be discussed further in the following sections (see Section 5.1.6 in particular).
Unsurprisingly, cancer incidence is also increasing at a faster rate in developing countries. While cancer rates do remain high in high-income countries (HIC), “...they are plateauing or decreasing for the most common cancers due to decreases in known risk factors, screening and early detection, and improved treatment…”.41 Meanwhile, a number of low- and middle-income countries (LMICs) are experiencing increased rates of these same cancers, particularly “...due to increases in smoking, excess body weight, and physical inactivity…” as well as lack of knowledge about risk factors, lack of early detection, and lack of high-quality treatment.42 LMICs also have a disproportionately high incidence of cancers stemming from infections, for example liver cancer, bladder cancer and cervical cancer (see below).4344
We have examined many of the different interventions in this area, many of which have the potential to be highly cost-effective but not all of which are under-funded at present or being carried out effectively by charitable organisations. We recommend vitamin A fortification as a method for reducing cancer morbidity and mortality which may be highly cost-effective, as well as both neglected and tractable.
5.1 Vitamin A fortification (stomach cancer)
As the second largest contributor to cancer morbidity and mortality, stomach cancer constitutes a sizeable portion of the total disease burden of cancer worldwide. It causes 841,000 deaths each year, as well as 17.9 million DALYs45 - that is, 1.53% of all deaths, and 0.73% of all DALYs worldwide (see Figure 4 below).46
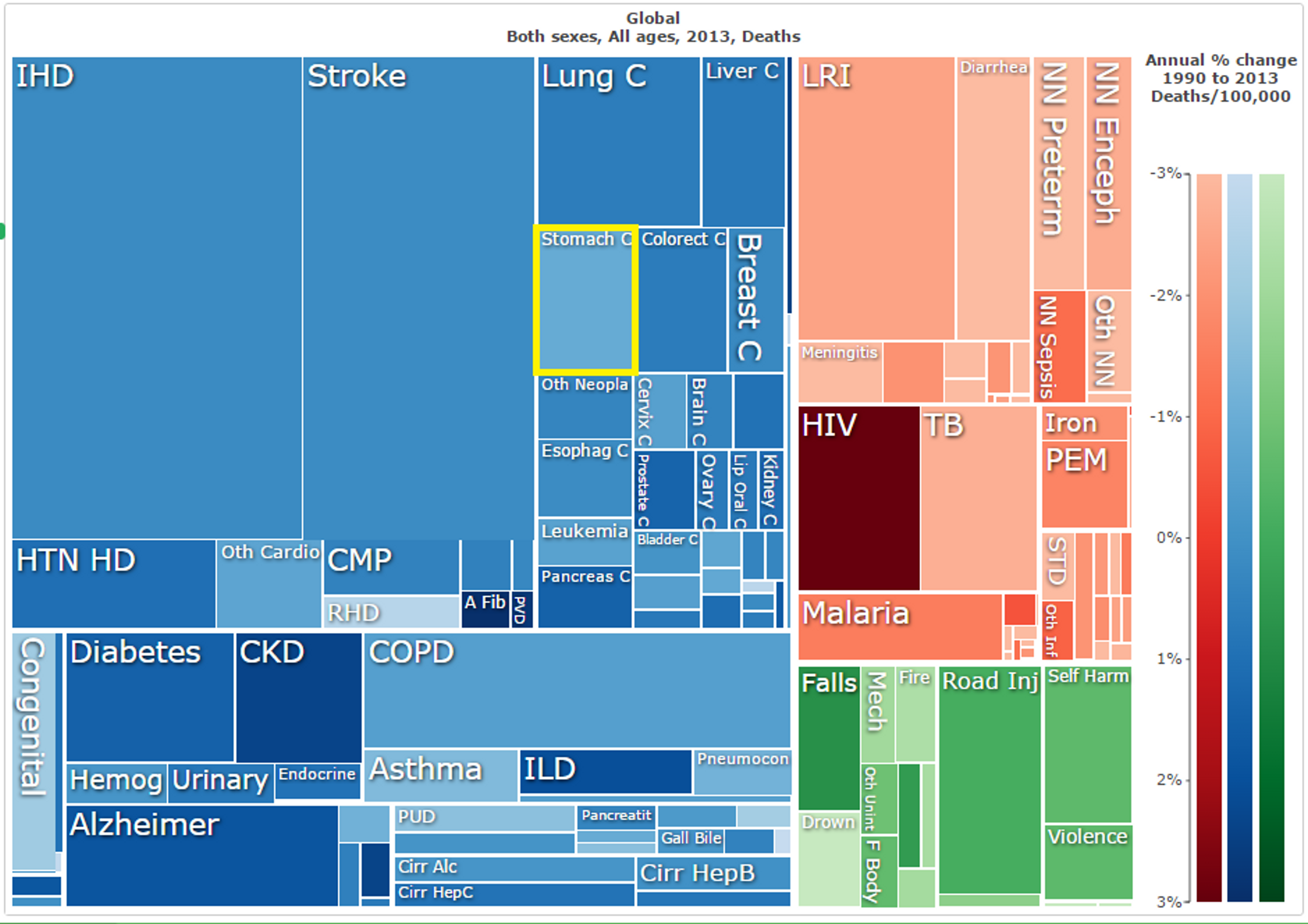
Figure 4: Stomach cancer (outlined in yellow) as a proportion of total global mortality in 2013;47
In addition, 600,000 of those deaths (71%) occur in developing nations, as do 77% of the DALYs incurred by stomach cancer.48 The United Kingdom’s National Health Service even describes it as “...a fairly uncommon type of cancer…”.49 This suggests that it may provide an opportunity for cost-effective interventions to improve health and decrease mortality in developing nations.
However, stomach cancer is typically only treatable through chemotherapy, radiotherapy, and surgery5051 which, in the United States, is at an average cost of more than $70,000 for the first year of treatment (and $4000/year thereafter).52
More promisingly, several prominent risk factors have been identified for stomach cancer, including high sodium intake,535455 ionising radiation,5657 high alcohol consumption,58 and exposure to tobacco smoke.596061
More recent research, including a meta-analysis of 47 different studies which spanned 1,221,392 human participants aged 18-98 years, has found that vitamin A deficiency is also a major risk factor, as it can cause DNA damage and thereby lead to the development of stomach cancers.626364656667 Thus, simply by supplementing the dietary intake of vitamin A in some regions and thereby reducing vitamin A deficiency, it may be possible to cost-effectively reduce the incidence of stomach cancer.
5.1.1 How does it work?
It is possible to improve the dietary intake of particular micronutrients, such as vitamin A, in LMICs by either directly providing vitamin supplements or by fortifying key products in the food supply. The latter is the far more cost-effective option - directly supplementing zinc, for example, costs more than five times as much as raising zinc intake through fortified foods.68
Micronutrient fortification, such as with vitamin A, can be performed during manufacture, and may be encouraged or mandated by national governments or company executives. The charity we recommend for this intervention, Project Healthy Children (PHC), also provides technical assistance to manufacturers and assists in training inspectors to continue to monitor the implementation of its fortification schemes.
5.1.2 Tractability and cost-effectiveness
It appears that micronutrient fortification is a highly cost-effective, and readily tractable, method of decreasing disease burden - from cancer specifically and also more widely. The issue of tractability is a minor one, as there are few major obstacles to establishing micronutrient fortification schemes in developing nations. This section will therefore focus mainly on the cost-effectiveness of implementing such schemes.
In regards to the efficacy of micronutrient supplementation, recent research has demonstrated that increasing micronutrient supplementation greatly decreases the risk of stomach cancer - vitamin A by 29%, vitamin C by 26%, and vitamin E by 24% (It is worth noting that the meta-analysis which produced this result included 1,221,392 human subjects aged between 18 and 98, and considered the effects of micronutrient supplementation over time-scales of between 1 and 14 years).69 In sub-Saharan Africa, vitamin A deficiency in particular is extremely prevalent, with up to 75% of preschool-age children affected by it in some countries70 (see Figure 5 below). Stomach cancer, while not constituting the majority of worldwide mortality, still kills 28,836 people per year in this region (and incurs 729,535 DALYs).71 Meanwhile, micronutrient fortification can be performed for approximately $0.07 per person reached by PHC,7273 so we can make a rough estimate of the cost of saving lives from stomach cancer. If vitamin A supplementation reduces the risk of stomach cancer by 29% then supplementing the entire population of sub-Saharan Africa may prevent 8,362 deaths and avert 211,565 DALYs, from the above. Theoretically, the total cost of doing so, through Project Healthy Children, would be approximately $68.87 million for entire sub-Saharan population of 988,088,000 74. Note that this estimate is merely to showcase how cheap micronutrient fortification is - currently not all people in sub-saharan Africa have access to staple foods that are produced on an industrial scale and that could be fortified at a such a low price. In other words, there will be diminishing marginal returns.
This initial estimate therefore begins to suggest that such an intervention would prevent deaths at an average cost of $8,236 per life saved and avert DALYs at an average cost of $326/DALY. In particular, these benefits are only due to stomach cancer and therefore exclude the majority of health benefits due to micronutrient fortification (see Section 5.1.3 below), which makes such estimates extremely impressive. After all, among the most cost-effective charities that we know of, it is considered extremely cost-effective to be able to improve health at a cost of approximately $2,838 per life saved and $78/DALY averted,75,76 and this is through the direct benefits rather than relatively small co-benefits such as cancer prevention.
However, there are several factors that make these estimates potentially overly optimistic. There are several mitigating factors:
- PHC may potentially not provide vitamin A fortification in all countries in which it is active (this turns out not to be the case - see Figure 5 below);
- The countries in which PHC is active (predominantly small countries in which nutrition is highly neglected) may not have rates of stomach cancer as high as the sub-Saharan average (again, this is not the case - see Figure 5 below);
- PHC may not be entirely responsible for the micronutrient schemes in the countries in which they operate, with other actors contributing, although this does not impact on the cost-effectiveness of micronutrient fortification overall (and the overall costs, which are fairly minor, are included in estimates of overall cost-effectiveness in the following section);
- Vitamin A fortification may not decrease the risk of stomach cancer for those already receiving sufficient vitamin A (the aforementioned meta-analysis may have predominantly considered populations with high levels of vitamin A deficiency) and, given this, the effectiveness of fortification may be restricted to only the portion of the population experiencing inadequate vitamin A intake;
| Country77 | Population78 | Vitamin A included? | Coverage | Stomach cancer mortality45 | Stomach cancer DALYs45 | Vitamin A deficiency in preschool-age children |
|---|---|---|---|---|---|---|
| Rwanda | 11,341,544 | ✔ | 80% | 276 | 6,971 | 6%79 |
| Malawi | 16,695,253 | ✔ | 80% | 127 | 3,748 | 60%80 |
| Liberia | 4,396,554 | ✔ | Unknown | 175 | 4,996 | >50%81 |
| Burundi | 10,816,860 | ✔ | ~80% | 333 | 8,855 | ~25%82 |
| Zimbabwe | 15,245,855 | ✔ | 80% | 322 | 6,693 | ~35%83 |
| Honduras | 7,961,680 | ✔ | Unknown | 783 | 16,755 | 14%84 |
| Sierra Leone | 6,315,627 | Very likely | Unknown | 286 | 8,850 | 75%85 |
| Nepal | 28,174,724 | Very likely | Low | 1,043 | 27,454 | ~30%86 |
| Tanzania | 51,822,621 | Very likely | Unknown | 1,105 | 27,453 | 24%87 |
Figure 5: National fortification programs to which PHC has contributed to date. Note that the fortification and supplement programs in Honduras (2000-2010), Rwanda(2007-present) and Malawi (2009-present)88 are now relatively well-established and PHC now only assists with the continuing monitoring of fortification. This may already contribute to lower incidence figures for vitamin A deficiency in these countries.
The above data addresses several of the above concerns: PHC’s programs do provide vitamin A fortification in all of the countries in which they currently operate, and are likely to do so in the three countries in which they are currently establishing new programs (Sierra Leone, Nepal, and Tanzania); and the rates of stomach cancer in the countries in which they operate are still quite high (particularly in Nepal and Tanzania, to which additional donations are most likely to contribute). In addition, we do believe that the national schemes contributed to by PHC are largely a product of their intervention due to the relatively small size and neglectedness of those countries. We also do not believe that the additional costs borne by local governments and other actors affect the cost-effectiveness estimates significantly as they are both fairly minor and are already taken into account by the overall cost-effectiveness estimates for improving general health which are considered in the following section. Also, the rates of vitamin A deficiency in the countries in which they operate are not a great deal lower than the 40% average for the developing world (in fact, the prevalence in Sierra Leone, Malawi and Liberia is far higher), so this does not reduce their cost-effectiveness more than comparable micronutrient fortification organisations.
Taking the above considerations into account, the estimates of $8,236/life and $326/DALY above are not likely to be inaccurate by more than one order of magnitude, but a more conservative estimate would likely be more accurate. The first improvement we can make, to produce a conservative estimate at least, is to replace the cost-per-person figure of $0.07 with a cost-per-country figure (from which the cost-per-person figure originates), for which $697,000 appears to be the maximum.89 Also, country-specific estimates of vitamin A deficiency can be used to conservatively estimate of what portion of the population will benefit, as this portion of the population will certainly be comparable to the control groups used in experiments.90 From this, as well as the above considerations, we are able to make the following estimates (albeit with a large degree of uncertainty due to incomplete and/or slightly outdated data):
- the fortification programs run by PHC result in deaths from stomach cancer being prevented at a rate of $24,220/death and avert DALYs at a rate of $920/DALY;
- if the relatively well-established programs are excluded, this drops to $19,100 per stomach cancer death averted and $720/DALY;
- in Tanzania in particular, PHC may save a life for every $11,330 spent and avert a DALY for every $460;
- and meanwhile, in some countries with well-established programs such as Rwanda and Malawi, the cost rises to $181,420 and $39,420 per death prevented, but this is likely due to the levels of vitamin A deficiency having already dropped substantially and therefore that the countries are warping overall data. (Other countries where PHC has begun to improve fortification rates may be doing so as well, but to a lesser extent and only in the direction of decreased cost-effectiveness, thereby simply producing a more conservative estimate.)
Given this, our best guess of the cost-effectiveness of stomach cancer prevention through the type of programs administered by PHC is $19,100/death averted and $720/DALY. However, this is still subject to a great deal of uncertainty and the true figure may be much higher or much lower.
When considered together with the wider benefits of vitamin A fortification on health beyond just cancer, this cost drops enormously - to less than $40/DALY (see the following section).
5.1.3 Positive wider impacts
The many other health benefits
There is extensive evidence of the wide-ranging health benefits of micronutrient fortification.91929394 Much of the total benefit provided is not, however, through the prevention of stomach cancer specifically, nor through the fortification of vitamin A in particular (as against iodine, zinc, folate and so on). This applies equally to PHC’s programs, which fortifies with a variety of micronutrients and which, of course, does not focus on stomach cancer specifically. When we include the co-benefits of other micronutrients and wider health impacts are included the cost-effectiveness of fortification improves greatly.
For example, deficiencies in vitamin A, iodine, iron, zinc, and folic acid contribute greatly to the prevalence and severity of the following conditions (see also Figure 6 below):
- iodine deficiency, which, by itself, accounts for 0.56% of all years lived with a disability in developing countries95 and which interferes greatly in mental development, causing an average loss of 6.9-10.2 IQ points in children under 5;96
- iron deficiency anemia, which makes up 6.76% of all years lived with a disability and 0.4% of all deaths in developing countries;97
- maternal hemorrhage, maternal sepsis and other maternal infections, which make up 0.17% of deaths and 0.19% of DALYs in developing countries and arise largely from iron deficiency;98
- diarrheal diseases, which makes up 2.96% of deaths and 3.51% of DALYs in developing countries, approximately 5-8% of which can be attributed to vitamin A deficiency and 3-5% can be attributed to zinc deficiency;99
- measles, which makes up 0.23% of all deaths and 0.39% of DALYs in developing countries, approximately 23% of which is attributed to vitamin A deficiency;100
- lower respiratory infections, which make up 5.18% of all deaths and 5.21% of DALYs in developing countries, approximately 2% of which is due to zinc deficiency;
- neural tube defects, which affect 320,000 newborns worldwide each year101 and which can be prevented by increasing maternal folic acid intake.102103
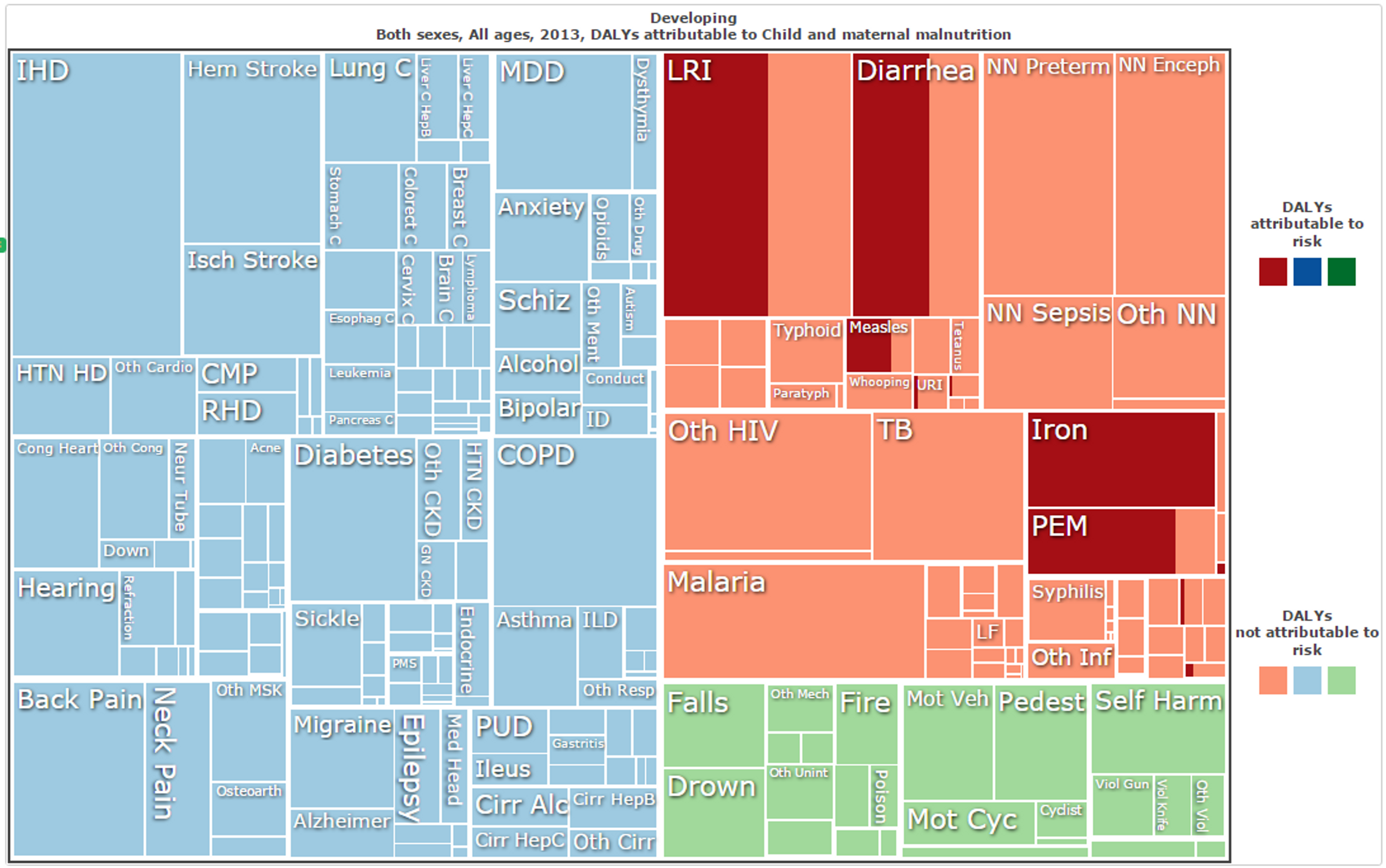
Figure 6: DALYs in all developing nations, with those attributable to child and maternal malnutrition (for all categories) shaded.104
It is estimated that 80% fortification coverage in Rwanda, Malawi, Zimbabwe and similar countries would result in: a 30% reduction in vitamin A deficiency; a 20% reduction in childhood anemia; a 30% increase in adult productivity; a 4-30% reduction in maternal mortality; and a 30% overall reduction in neglected tropical diseases such as schistosomiasis.105106107 Research has indicated that vitamin A fortification improves health at a cost of less than $40/DALY averted in many areas,108109110 and some estimates place this cost as low as $11 in Malawi and $31.78 in Zimbabwe (both specifically for wheat flour).111 In other countries, it has been found that micronutrient fortification (including nutrients other than vitamin A) can produce health benefits for as little as $2/DALY (in Nigeria), $3/DALY (Democratic Republic of Congo), $4/DALY (Myanmar), and less than $100/DALY in more than 30 different developing countries.112113 PHC operates in several of these, as listed below in Figure 7, and we believe that these approximations are reasonably accurate to the total costs incurred by PHC’s programs.114
All of these estimates, however, do not include the benefits provided through stomach cancer prevention, and hence may be even lower.
| Rank | Country | Food | Total cost (US$) | Cost per DALY averted (US$) |
|---|---|---|---|---|
| 16 | Malawi | wheat | 1,344,446 | 25 |
| 21 | Zimbabwe | sugar | 2,218,527 | 33 |
| 30 | Zimbabwe | wheat | 1,872,396 | 43 |
| 46 | Rwanda | oil | 6,623,699 | 68 |
| 47 | Sierra Leone | oil | 10,601,950 | 69 |
| 52 | Malawi | oil | 9,738,123 | 105 |
| 54 | Burundi | oil | 5,500,917 | 106 |
Figure 7: Cost-effectiveness rankings of the countries in which PHC is active (and products which they fortify), taken from a table of 60 different countries’ micronutrient interventions, and arranged by the cost per DALY averted.115
Continuation of programs into the future
For policy-based and manufacturing-based fortification programs such as that implemented by PHC, the benefits for local populations continue long after they are implemented. Unless government policy or manufacturing process changes (which is unlikely due to the extremely low cost of the programs), foods will continue to be fortified indefinitely into the future, thereby potentially providing fortification to a greater number of people in future generations. It also means that the health benefits will aggregate year upon year, so the cost per death prevented ($19,100 from stomach cancer alone) will decrease enormously when considered over the span of several decades. Even just over 10 years, which seems quite a conservative estimate of how long the programs might stay in place after PHC establishes them, the cost-effectiveness might improve to $1,910/death prevented ($2,180 at a 3% p.a. discount rate). However, this does not include the relatively minor costs of ongoing monitoring and follow-ups, so should not be considered an accurate estimate but instead merely illustrative.
5.1.4 Due diligence: Possible offsetting/negative impacts
Over-consumption of micronutrients
It seems plausible that delivering micronutrients through fortification rather than direct supplementation may put some of the population at risk of consuming excess amounts, and potentially experiencing adverse health effects.
This intuition does indeed hold true in extreme cases, specifically for stomach cancer prevention, when vitamin A intake greatly exceeds the tolerable upper intake,116 but we are quite confident that PHC’s fortification efforts will result in neither a significantly greater prevalence of such high intake nor a degree of negative health effects which compare to the positive effects described in Sections 5.1.2 and 5.1.3.
In particular, such adverse effects are extremely unlikely to occur when sufficient prior research is performed. For instance, before implementing fortification programs in a new country, PHC consults existing nutrition and food consumption surveys (and also conducts their own) in order to establish the optimal level of fortification, including which nutrients are not required, therefore minimising the risk of adverse health effects.117118
Also, regardless of whether fortification is tailored to particular countries, PHC’s programs result in levels of fortification which are well within safe limits.119120 There is a great deal of evidence supporting the overwhelmingly positive effects of fortification at levels such as these, including extensive meta-analyses.121122123124 Given this, we do not believe that this reduces the cost-effectiveness of micronutrient fortification, or the activities of PHC, by a considerable amount.
Discounting future benefits
Whether to discount lives saved (or DALYs averted) with time is a controversial moral question. Despite this, if this is done at any rate (e.g. 3%p.a. as is the standard rate used by economists), the benefits of micronutrient fortification may be somewhat mitigated.
When simply aggregating the lives saved over time, it is unlikely that this will be a considerable problem, as we have not considered the long-term benefits in our calculations in Section 5.1.2 and, therefore, the total benefits will be greater than we have already supposed whether a discount rate is applied or not. As mentioned briefly in Section 5.1.3 above, the total impacts over 10 years are reduced by less than 15% when a 3% discount rate is applied. Over 100 years the reduction becomes approximately 68% but, still, we have not considered effects this far into the future in our analysis so the true total benefits are likely much higher than we have estimated, even if the value of future benefits is discounted in this way.
A greater concern is that the delay between fortification and the prevention of stomach cancer deaths may be quite a long time, and that therefore even the initial benefits may be subject to heavy discounting. After all, the average age of those diagnosed with stomach cancer is 69125 and vitamin A deficiency primarily affects children and expectant mothers. Nonetheless, the primary meta-analysis on which our cost-effectiveness estimate is based does not include any studies conducted over a time-scale greater than 14 years, and many much shorter (as well as subjects aged from 18 to 98 years, all of whom could be expected to benefit from fortification).126 At a discount rate of 3%, even if all of the benefits take an entire 14 years to occur (which is almost certainly a considerable overestimate), this reduces the value of those benefits by only about 33%. It also does not include the much broader and much more immediate benefits of reducing child mortality, maternal mortality and micronutrient deficiencies. Thus, we do not believe that discounting greatly reduces the cost-effectiveness of micronutrient fortification for reducing cancer incidence.
Uncertainty
This is likely the single greatest problem for fortification programs. In our calculations of cost-effectiveness, there is a great deal of uncertainty and it is hence entirely possible that the health benefits of micronutrient fortification are less than we estimate, both for stomach cancer prevention and for health in general. For instance, the causes of stomach cancer are numerous, and the predicted 29% reduction may vary greatly by country or according to other factors. The estimates of prevalence of vitamin A deficiency across populations may also be inaccurate, with some sourced from studies conducted in 2011 (see Figure 5 above). To a lesser extent, the wider impacts of micronutrient fortification are somewhat uncertain, with estimates of child mortality reduction varying from more than 30% to 11% and below.127 We are extremely confident that micronutrient fortification will have a net positive impact, though it is possible that our estimates of the exact extent of the impact are not wholly accurate. Still, the cost-effectiveness estimates which we have made above are still ‘best guesses’ of the true cost-effectiveness, based on some fairly conservative assumptions.
5.1.5 Neglectedness
Micronutrient fortification and supplementation is a relatively neglected intervention area, particularly in the areas which are the focus of PHC’s activities.
There are other charities and other organisations working on micronutrient fortification (of vitamin A in particular) including the Global Alliance for Improved Nutrition,128 the Golden Rice Project,129 Vitamin Angels,130131 the Iodine Global Network,132133 and UNICEF.134
Still, despite the potential for cost-effectively obtaining major health benefits, in general, nutrition is still severely underfunded. Compared to other health interventions (such as for HIV/AIDS) as well as to emergency food aid (see Figures 8 and 9 below).
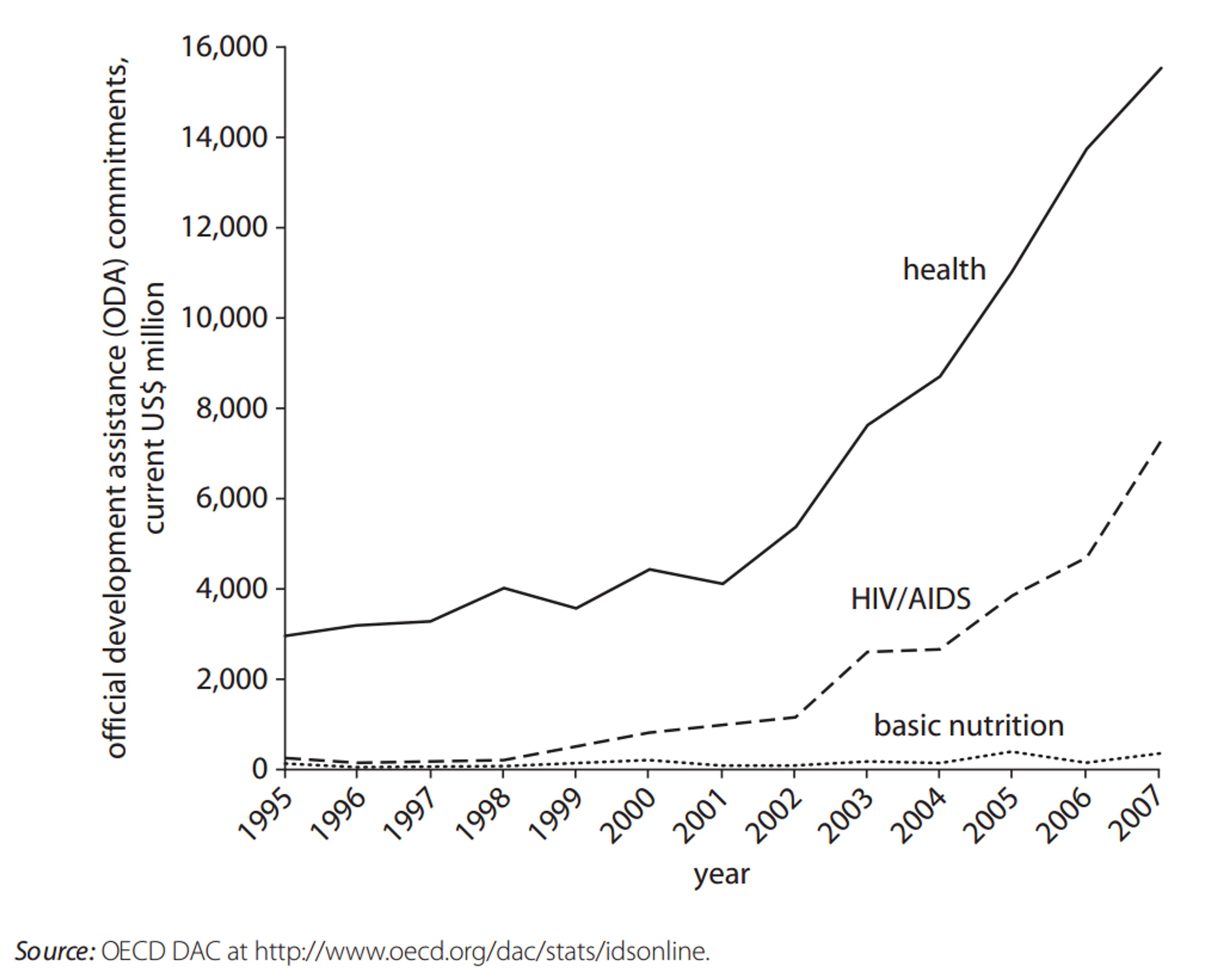
Figure 8: Official Development Assistance Commitments for Health, HIV/AIDS, and Nutrition, 1995–2007.135

Figure 9: Official Development Assistance Commitments for Nutrition and Emergency Food Aid, 1995–2007.[137]
In addition, vitamin A deficiency remains extremely high in many developing countries,136 producing extremely high disease burdens in some areas.137 In many more countries, adequate fortification programs have yet to be established.138 Both of these facts hold true of numerous nations across sub-Saharan Africa, including Zimbabwe, Burundi, Sierra Leone, Liberia and a large number of other countries to which PHC could scale their operations in future. In particular, PHC generally focuses their efforts on relatively small countries in which severe nutritional deficiencies are prevalent, thereby having a greater marginal impact.139140141
Meanwhile, a study from the World Bank has estimated that an additional $10.3 billion could be productively used each year to scale up nutrition interventions142 - an estimate which has largely been confirmed elsewhere.143 The indicates that fortification as a whole is still a sufficiently neglected area.
In particular, the World Bank has estimated that, for technical assistance, initial subsidies for fortificant and social marketing, an additional $1 billion is required, as well as $200 million for monitoring, evaluation and operations research.144 These are precisely the areas on which PHC works, therefore indicating that the area of their work is sufficiently neglected to allow for the marginal impacts of donations to remain high. Given this, we are quite confident that the micronutrient fortification work performed by PHC is otherwise quite neglected, despite the presence of other charities.
5.1.6 Charity recommendations
Project Healthy Children

Donor fit
International development, public health and cancer prevention
What do they do?
Project Healthy Children (PHC) works with local governments and manufacturers to fortify staple foods such as flour, sugar, rice and oil. The process adds micronutrients such as folic acid, iodine, iron, vitamin A and zinc in order to tackle micronutrient deficiency. This follows a comprehensive “country assessment” before they begin operations, including surveys of health and nutrition, consumption patterns, food imports, and the political environment. Based on these assessments, PHC identifies the best foods to fortify and the micronutrients which are most needed. They then then provide technical assistance to governments in designing and implementing fortification programs, and in drafting national fortification standards, as well as technical assistance to manufacturers and inspectors to ensure that highly effective methods and monitoring systems are used.
Overall evaluation
Project Healthy Children is a highly cost-effective charity, and has previously been evaluated as such by Giving What We Can.145 A large volume of evidence supports the efficacy and cost-effectiveness of PHC’s activities, and monitoring indicates that PHC’s work to date has been highly effective. In addition to greatly improving general health at a rate of less than $40/DALY, we also believe that PHC is able to prevent a death due to stomach cancer for approximately every $19,100 donated.
Cost-effectiveness [⚫⚫⚫⚫⚫]
Cost-effectiveness (specifically for cancer prevention) [⚫⚫⚫⚪⚪]
Robustness of evidence [⚫⚫⚫⚫⚪]
Robustness of evidence (specifically for cancer prevention) [⚫⚫⚫⚪⚪]
From Sections 5.1.2 and 5.1.3 above, we are quite confident that PHC’s activities are indeed highly cost-effective in improving health in the countries in which they operate. We also have reason to believe that they are also cost-effective, to a lesser degree, specifically for the prevention of stomach cancer. We estimate that donations to PHC improve general health at a rate of less than $40/DALY averted, and this claim is supported by a considerable body of evidence.
Specifically for stomach cancer, we estimate that donations to PHC may potentially save lives for approximately $19,100/life and reduce disease burden at a rate of $720/DALY, although these estimates are subject to a large degree of uncertainty and there is less evidence for this effect than for the general benefits of micronutrient fortification. Still, this compares favourably to the other cancer interventions for which there is currently a funding gap (see the following sections) and we therefore recommend donating to PHC as an opportunity to cost-effectively reduce cancer morbidity and mortality.
Quality of implementation [⚫⚫⚫⚫⚪]
We are impressed with the quality of PHC’s implementation of programs so far, and their success to date in number of countries. The policy and institutional changes that PHC has accomplished in many countries give clear indications that they have been highly successful.146147148 In addition, PHC’s evaluation and monitoring activities have also demonstrated that implementation in these countries has so far been quite successful,149 and believe that such monitoring leaves only a very low probability that their programs are not having a substantial impact.
Room for more funding (✔)
As of September 2015, PHC held about $200,000 in reserves,150 which translates to about 3-4 months of operational costs, which we think is not excessive. Thus, in the short-term there is room for more funding. PHC has told us that with additional funding they would intensify their monitoring efforts, which is one of the most critical components to any national fortification program. In the longer term, based on PHC’s development plan, we expect that PHC could productively use an additional $2.5 million to further expand its programs.
Also, in comparison to other organisations working on micronutrient fortification, PHC does appear to have more room for additional funding. For instance, the Iodine Global Network received approximately $500,000 in funding from USAID in 2015151 and the Global Alliance for Improved Nutrition (GAIN) has received funding from the Bill and Melinda Gates Foundation through mid-2015, which may also be renewed.152 Moreover, PHC is only active in small African countries with small populations (<17 million), whereas GAIN is not currently active in these countries.153 This supports the claim that donations made to PHC will have a greater marginal impact than donations made to other charities in the same area.
See Part 2 for our analysis of other prevention and treatment interventions.
- *[^fn-1]: "What Is Cancer? - National Cancer Institute." 2015. 8 Feb. 2016 <http://www.cancer.gov/about-cancer/what-is-cancer>